Diabetic retinopathy
Description:
Diabetic retinopathy is one of the possible complications of diabetes, and reflects general lesions. Its evolution can lead to complete blindness if not treated properly.Retinopathy can appear after a few years of diabetes and will be aggravated by factors such as the duration people have had diabetes for and its poor balance, arterial hypertension, tobacco, cholesterol and triglycerides.
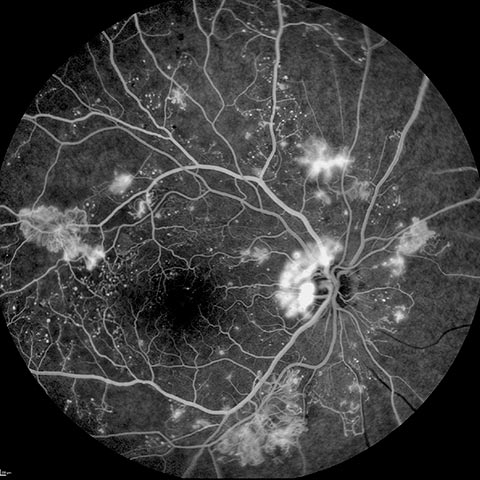
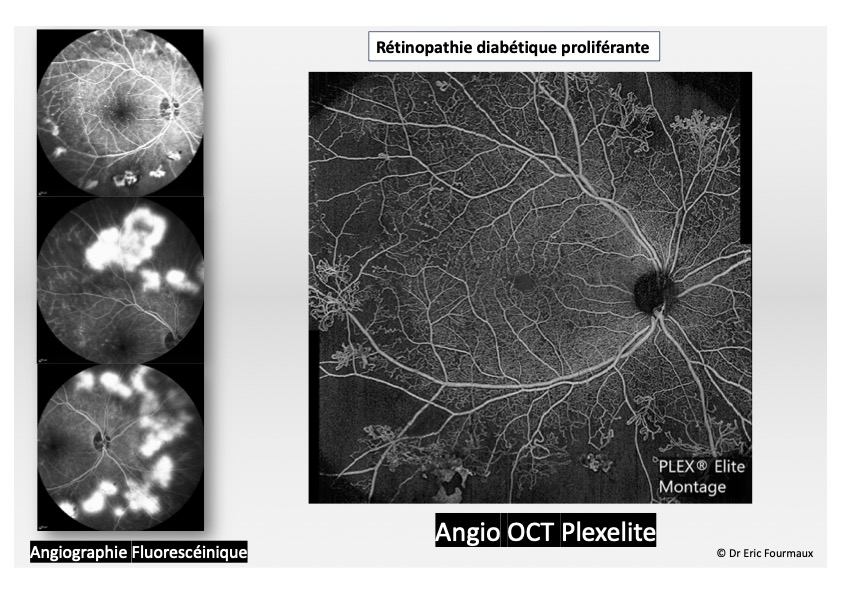
Diabetic retinopathy has several stages of growing seriousness. It is characterized by lesions affecting retinal capillaries causing a retinal oedema, haemorrhage and the proliferation of abnormal blood vessels.
Download the brochure
Symptoms:
At the beginning of a diabetic retinopathy, the patient experiences no symptoms and the vision is preserved. A yearly fundus examination is necessary to detect the disease in this early stage and evaluate its potential general impact. At the next stage, a brutal or gradual loss of visual acuity signals the appearance of complications of variable gravity such as a macular oedema which impedes central vision, intravitreous haemorrhage or retinal detachment.Fundus examination coupled with retinophotography is the main examination allowing to detect diabetic retinopathy at its various stages or the presence of a macular oedema (central) in order to guide the treatment.
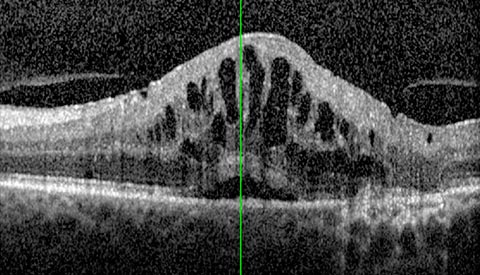
A macular OCT (Optical Coherence Tomography) allows to identify a macular oedema and to follow its response to the treatment.
Treatment:
In parallel to restoring the balance of diabetes and arterial hypertension, the treatment of diabetic retinopathy consists of treating the affected areas of the eye by laser. Some complications will need surgery.At an early stage, diabetic retinopathy requires no specific treatment. However, a strict control and balance of diabetes and of other risk factors such as arterial hypertension and lipid profile are necessary to control its progression.
At a later stage, various treatments are required:
- Laser photocoagulation: several sessions spaced at various intervals depending on the condition’s seriousness. This treatment aims at destroying non-vascularized ischemic areas in the peripheral retina, in order to allow a better blood irrigation of central retina and thus avoid the development of abnormal vessels or newvessels (which might cause a retinal detachment or intraocular haemorrhage).
- Laser is also used to treat localised macular oedema.
For these different treatments we benefit from last generation multisport micropulse lasers, which are quicker, more comfortable and more efficient.
- Intraocular injections of corticoids or anti-VEGF in case of a generalized macular oedema. Repeated injections are often necessary.
- In case of a tractionnal macular oedema causing intravitreous haemorrhage or in case of a retinal detachment, the prescribed treatment is surgery (posterior vitrectomy).

 Book an appointment
Book an appointment