Vein occlusions
Retinal vein occlusions (RVOs) are a common vascular disorder of the eye. They involve occlusion of one or more of the 4 retinal venous drainage branches (RVBs), or in the most serious cases, occlusion of their central trunk (RVO). This occlusion, which usually occurs suddenly, is linked to the formation of a venous clot that causes upstream leakage of plasma fluid and red blood cells into the retinal tissue concerned, leading to edema and reduced visual acuity if the macula is affected. In the most severe forms, occlusion can lead to ischemia and cell death in the occluded area.
If the clot does not dissolve rapidly, it causes more or less irreversible damage to the veins concerned, leading to their hyperpermeability.
The cause of retinal vein occlusions is multifactorial. After the age of 50, they most often occur in the context of chronic cardiovascular problems, hyperlipidemia, diabetes, sleep apnea syndrome or, in ocular terms, glaucoma with hypertonia. Their onset may be triggered by an episode of dehydration that decompensates the situation.
In young people, the causes are more often linked to coagulation factor disorders or the use of oral contraception.
In the event of venous occlusion, all these factors must be investigated by the appropriate practitioners.
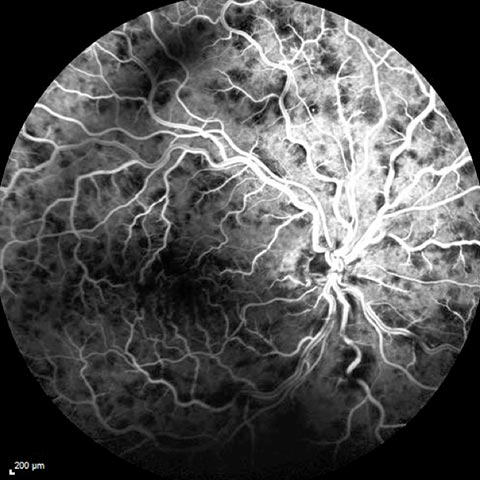
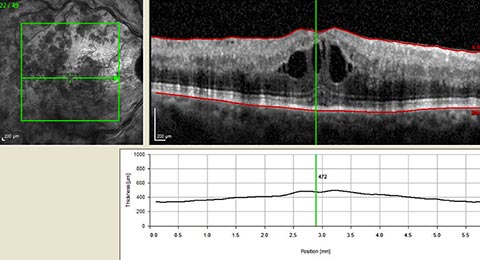
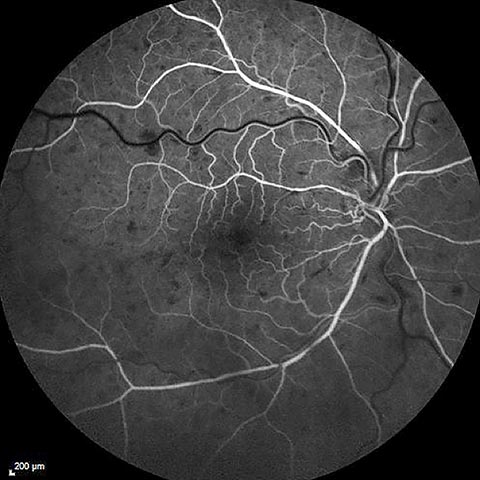
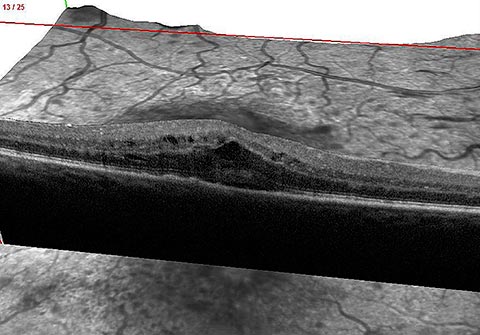
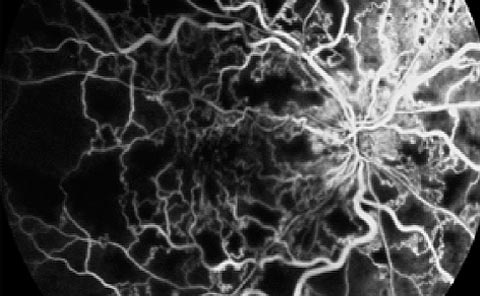
Ophthalmological diagnosis of occlusion and assessment of its severity are based on fundus examination, fluorescein angiography and/or Angio-OCT and macular OCT. These examinations are repeated during follow-up, depending on progress.

Treatment
General treatment is based on the management of any causal factors and, from an ophthalmological point of view, the consequences of occlusion, i.e. edema and ischemia. There is no treatment that can directly dissolve the clot in the retinal veins.
Retinal macular edema is treated with intraocular injections of anti-VEGF, which are repeated as the condition progresses, or with intraocular injections of sustained-release corticosteroid implants. These treatments usually result in significant visual recovery, but may take several years.
Peripheral retinal ischemia is treated with laser photocoagulation to avoid secondary complications such as intravitreal hemorrhage or neovascular glaucoma.
In the event of ischemia and cell death in the central reading area (macula), visual loss is irreversible.