Macular hole
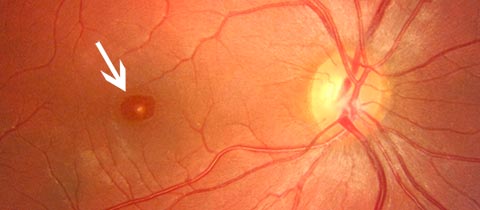
The macular hole is most often visible on fundus examination.Approximately 1mm in diameter, it is responsible for fine, precise vision and, in particular, for reading.Macular damage leads to reduced visual acuity, image distortion (metamorphopsia) and changes in object size and color.The macular hole is a loss of retinal substance.This hole most often occurs spontaneously after the age of sixty, but may more rarely affect younger patients, particularly in cases of high myopia or after trauma.
Symptoms
Symptoms are moderate in the early stages when the macular hole is small.
If left untreated, the diameter of the macular hole will gradually increase, leading to a functional handicap that can become major, with loss of central vision making reading impossible.
However, the peripheral visual field is preserved, and the macular hole does not lead to blindness in the affected eye.
The macular hole is caused by posterior vitreous detachment.
The vitreous is a transparent gel that fills the ocular cavity and adheres strongly to the retina.
From around the age of sixty, this vitreous changes and eventually detaches from the surface of the retina. More often than not, this process occurs unhindered, but in a few cases, when adhesion is too strong, this traction leads to the formation of the macular hole.
Diagnosis
The macular hole is most often visible on fundus examination. Color photography (retinography) is useful for comparing pre- and post-operative aspects. But it’s optical coherence tomography (OCT) that provides the most precise information (hole diameter, retinal thickness, vitreous condition…) and enables post-operative evolution to be followed perfectly.
Treatment
Treatment is surgical. The aim of the surgery is to obtain closure of the macular hole and therefore a functional improvement, but the operated eye will not be able to recover all of its capabilities. The visual cells lost during the formation of the hole cannot be reconstituted.
The operation is usually performed under local anaesthetic.
The vitreous body is removed (vitrectomy), and a thin membrane is peeled off the surface of the retina (internal border).
At the end of the procedure, a gas is injected into the eye to help reapply the edges of the hole.
This gas resolves spontaneously in around 15 days, and is gradually replaced by aqueous humor secreted by the eye.
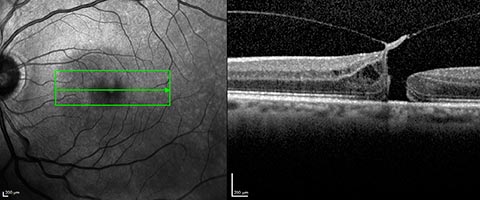
Pre-op appearance
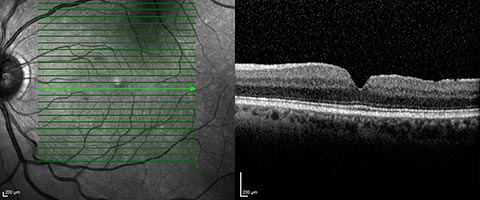
Post-operative aspect
Hospitalization:
The procedure is carried out under local anaesthetic, and can be performed on an outpatient basis. Patients living alone or too far from the surgical clinic may benefit from a short hospital stay.
Evolution
Post-operative course:
Usually painless.
A slight sensation of a foreign body may be felt for the first few days.
The patient must maintain a face-down position (known as the “bubble position”) for 18 to 20 hours a day, for 2 to 5 days depending on the case.
Strict adherence to this position is essential for recovery.
Post-operative treatment is limited to eye drops.
Air travel or stays in the mountains at altitudes of over 1,000 metres are contraindicated as long as gas remains in the eye.
Functional results:
Surgery closes the macular hole in over 95% of cases.
Vision improves progressively over several months, and final recovery depends on the size and age of the macular hole.
In patients who have not yet undergone cataract surgery, lens opacification may occur a few months after vitrectomy.
An intervention may therefore be necessary to regain the visual benefit obtained after macular hole surgery.
Complications :
Complications are rare, but can occur as after any surgery.
- The risk of infection is around 2 per 1000. Infection can be effectively treated with an intraocular injection of antibiotics, but can sometimes lead to severe loss of visual function or even loss of the eye.
- Retinal detachment. This occurs in around 1 in 100 cases, usually within three months of surgery. It requires further surgery.
- Elevated intraocular pressure or excessive inflammatory reaction requiring adaptation of local, eye-drop or general treatment.
Conclusion :
The results of this surgery are good in the vast majority of cases, with very satisfactory functional recovery.
In the case of large, old macular holes, however, results may be limited.



