Diabetic retinopathy
Diabetic retinopathy is one of the complications of diabetes, reflecting generalized lesions. Its insidious evolution can lead to blindness if left untreated.
Retinopathy may appear after a few years, with aggravating factors such as long-standing and poorly controlled diabetes, hypertension, smoking, and cholesterol and triglyceride disorders.
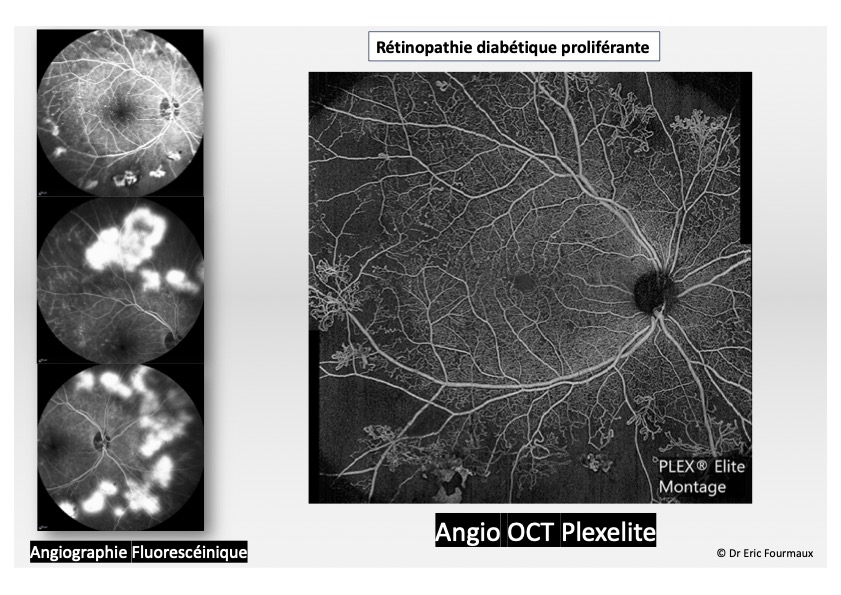
Diabetic retinopathy comprises several stages of increasing severity. It is characterized by lesions affecting the retinal capillaries, which will be responsible for retinal edema, hemorrhages and the proliferation of abnormal vessels.
Symptoms
At the onset of diabetic retinopathy, no symptoms are felt by the patient, and vision is preserved. A systematic annual fundus examination is necessary to detect these early stages and assess the possible general impact of the disease. At an advanced stage, a sudden or progressive drop in vision indicates the onset of complications of varying severity, such as macular edema (which reduces central vision), intravitreal hemorrhage or retinal detachment.
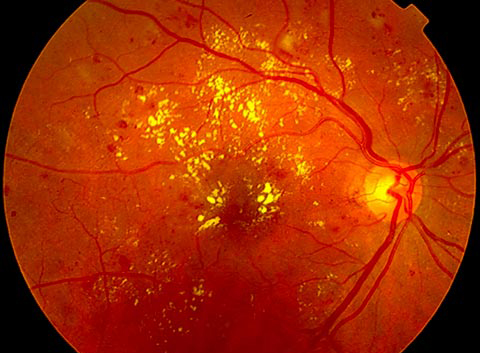
Fundus examination, supplemented by retinophotography, is the main screening test for identifying the different stages of diabetic retinopathy, or the presence of (central) macular edema, in order to guide treatment.
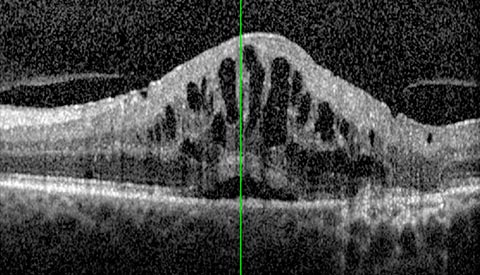
Macular OCT (Optical Coherence Tomography) can be used to detect macular edema and monitor response to treatment.
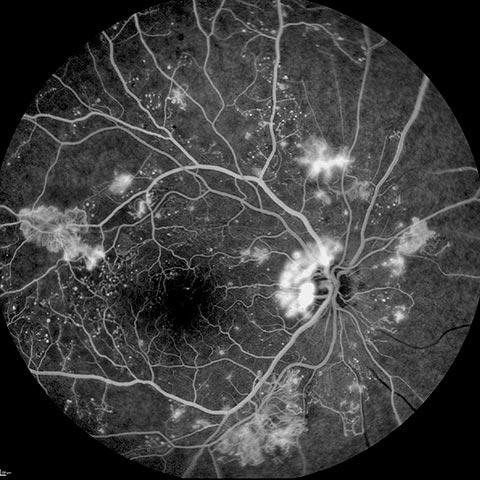
Fluorescein angiography (fundus photography with injection of a fluorescent dye) or wide-field OCT angiography can be performed to detect macular or peripheral ischemia and guide laser treatment.
Treatment
In addition to balancing diabetes and hypertension, diabetic retinopathy is treated by laser therapy. Some complications require surgical intervention.
In its early stages, diabetic retinopathy requires no specific treatment. However, strict control of diabetes and other cardiovascular risk factors, such as hypertension and lipid levels, is essential to limit its progression.
In the advanced stage, various treatments are used
- Laser photocoagulation in several sessions at variable intervals, depending on the severity of the retinopathy. The aim of this treatment is to destroy non-vascularized ischemic areas of the peripheral retina in order to improve irrigation of the central retina and prevent the development of abnormal vessels or neo-vessels that could lead to retinal detachment or intra-ocular hemorrhage.
- The laser is also used to treat localized macular edema.
For these different treatments, we use the latest-generation multi-spot micropulse laser, which is much faster, more comfortable and more effective.
- Intraocular corticosteroid or anti-VEGF injections for diffuse macular edema. Repeated injections are often necessary.
- Surgery with posterior vitrectomy is indicated in cases of tractional macular edema, intravitreal hemorrhage or retinal detachment, particularly tractional.

