AMD
AMD is the leading cause of legal blindness (visual acuity less than 1/10) in France among people over 50.
Left untreated, this disease can lead to the irreversible destruction of the central area of vision known as the macula. The peripheral retina is still respected, which means that we can continue to move around and remain relatively independent.
Symptoms
The clinical signs are a distortion of straight lines, which are seen as wavy, reduced vision and the perception of dark spots in the central field of vision.

There are 2 clinical forms, which may occur separately or in combination:
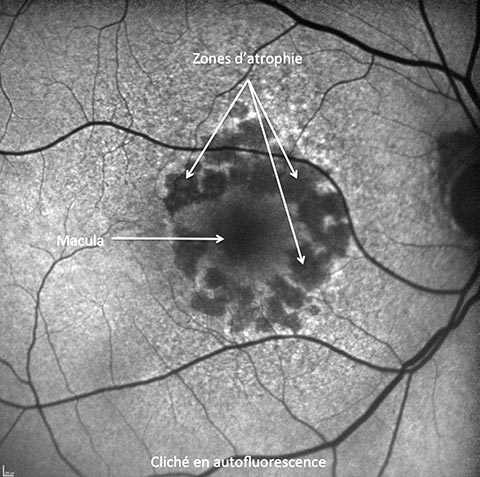
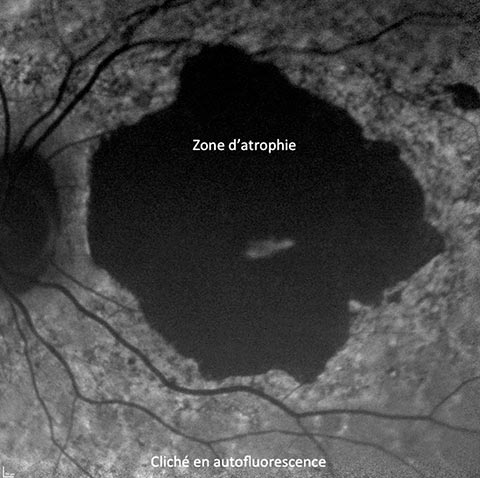
The atrophic or “dry” form:
This consists of progressive and irreversible atrophy of the central retina, leaving an island of vision for a long time. This form of AMD evolves slowly, but has no recognized, effective treatment apart from dietary supplements containing Lutein and Omega 3, which can slow its progress. Smoking cessation and the wearing of sunglasses can reduce the risk and slow the progression of the disease. New treatments in the form of intravitreal injections are currently being developed, and could help slow the progression of this atrophy in the years to come.
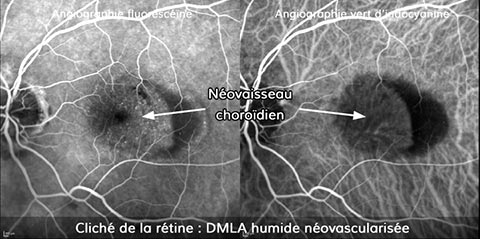
The exudative or wet form:
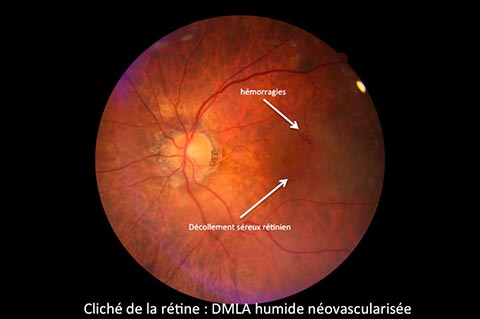
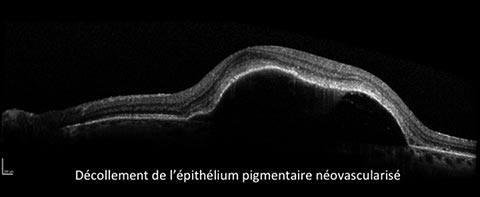
This follows the development of abnormal vessels under the central retina, linked to the aging of retinal and sub-retinal structures. These neovessels grow rapidly. Their structure, which is permeable to blood fluids, is responsible for the accumulation of these fluids in or under the retina. They can also rupture and bleed under the retina.
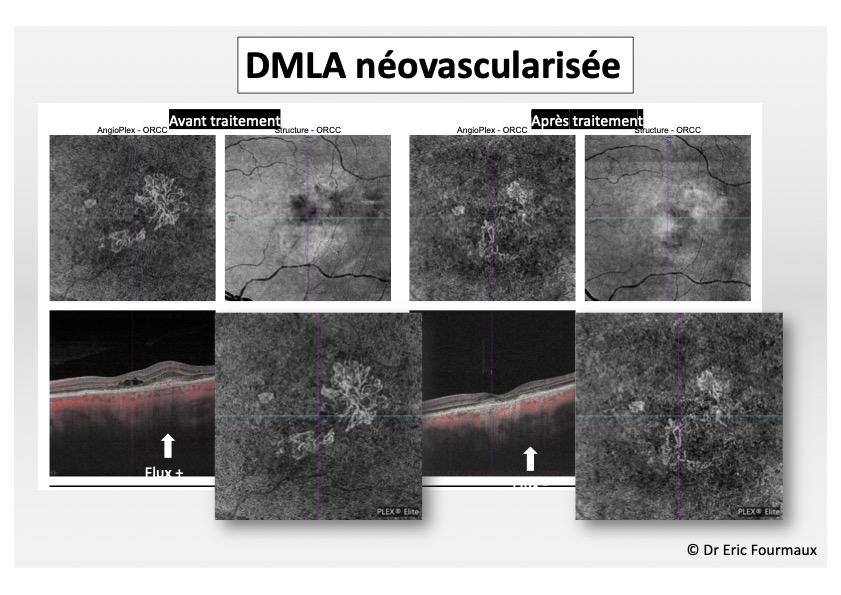
Diagnosis is based on a fundus examination, OCT and Angio OCT to identify abnormal vessels and assess their impact on the retina. In certain cases, fluorescein and indocyanine green angiography may be necessary to clarify the diagnosis, after antiallergic preparation and in the absence of serious contraindications.
Treatment
Treatment involves the use of a pharmaceutical molecule from the anti-VEGF family. Several types of molecule are now available. This drug is administered endocularly by intravitreal injection. Its aim is to heal the abnormal vessel, stop its progression and eliminate sub- and intra-retinal fluid leaks, thereby improving visual acuity. The neovessel scar itself can sometimes limit visual recovery if it lies below the center of the reading area.
These injections are performed in a specially adapted outpatient room. They are preceded by a local anaesthetic and disinfection of the eye. The injection is made with a very fine 30 gauge needle at a precise point that is safe for the eye. It is not very painful and lasts only a few seconds.
An initial series of several injections every month, depending on the molecule and clinical response to treatment, is initially prescribed until retinal fluid leaks disappear, macular anatomy is restored and visual improvement is achieved. In the majority of cases, further injections are then required at a patient-specific pace to maintain visual acuity gains, as the disease is chronic.
The most frequent incidents following this injection may be the occurrence of a subconjunctival hemorrhage (white of the eye), which is not serious and resolves within a few days, or the visualization of small black dots for 24 hours due to the presence of sterile air bubbles in the injected product.
Very rarely, ocular hypertonia (a sensation of transient visual loss immediately after injection) may occur, and should be reported to your doctor. Endocular infection, intravitreal haemorrhage or retinal detachment may occur very exceptionally.
In the event of a recent (less than 3 months) myocardial infarction or stroke, it is important to inform your doctor, who will discuss with you the best time for the injection.
In certain specific forms of AMD, dynamic verteporfin phototherapy may be proposed. Vitreoretinal surgery is exceptionally reserved for cases of heavy bleeding under the macular retina.